Authors: Barry A. Finette, Megan McLaughlin, Samuel V. Scarpino, John Canning, Michelle Grunauer, Enrique Teran,
Marisol Bahamonde, Edy Quizhpe, Rashed Shah, Eric Swedberg, Kazi Asadur Rahman, Hosneara Khondker, Ituki Chakma, Denis Muhoza, Awa Seck, Assiatta Kabore, Salvator Nibitanga, and Barry Heath
American Journal of Tropical Medicine & Hygiene
Received October 30, 2018. Accepted for publication March 11, 2019. Published online April 15, 2019.
Abstract. Approximately 3 million children younger than 5 years living in low- and middle-income countries (LMICs)
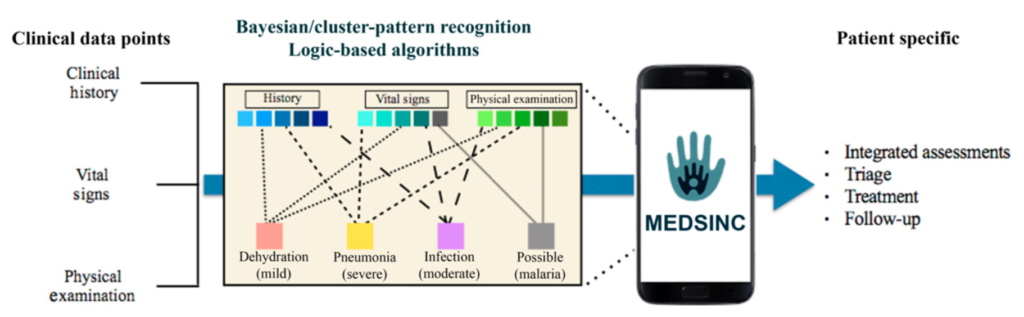
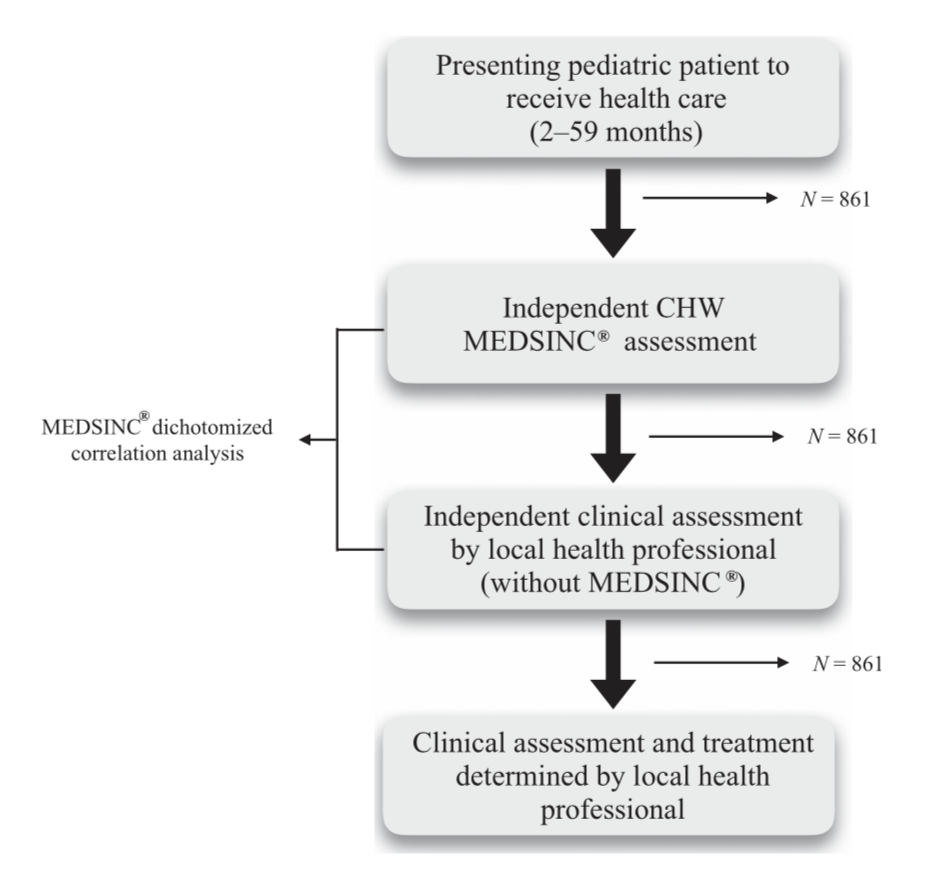
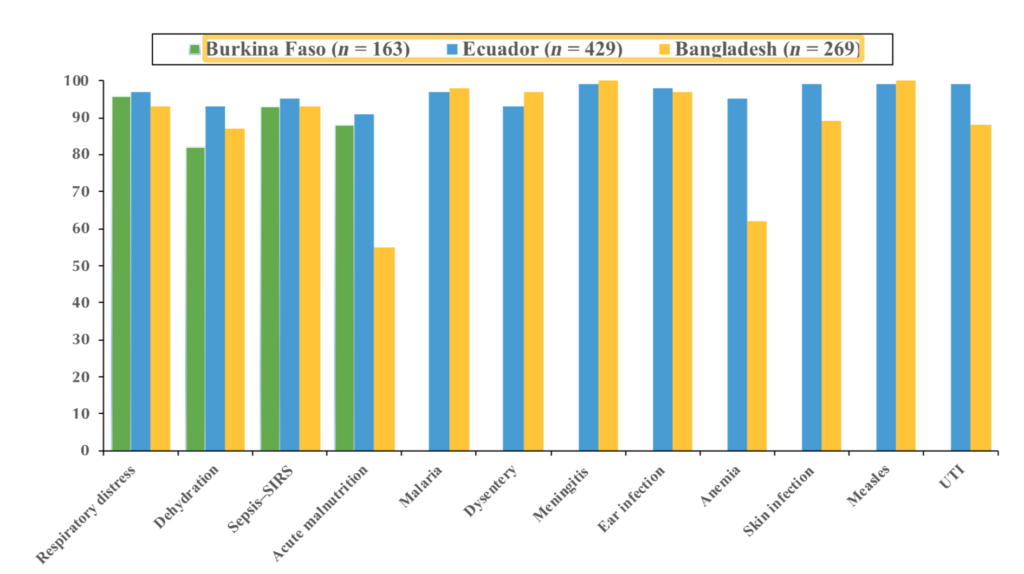
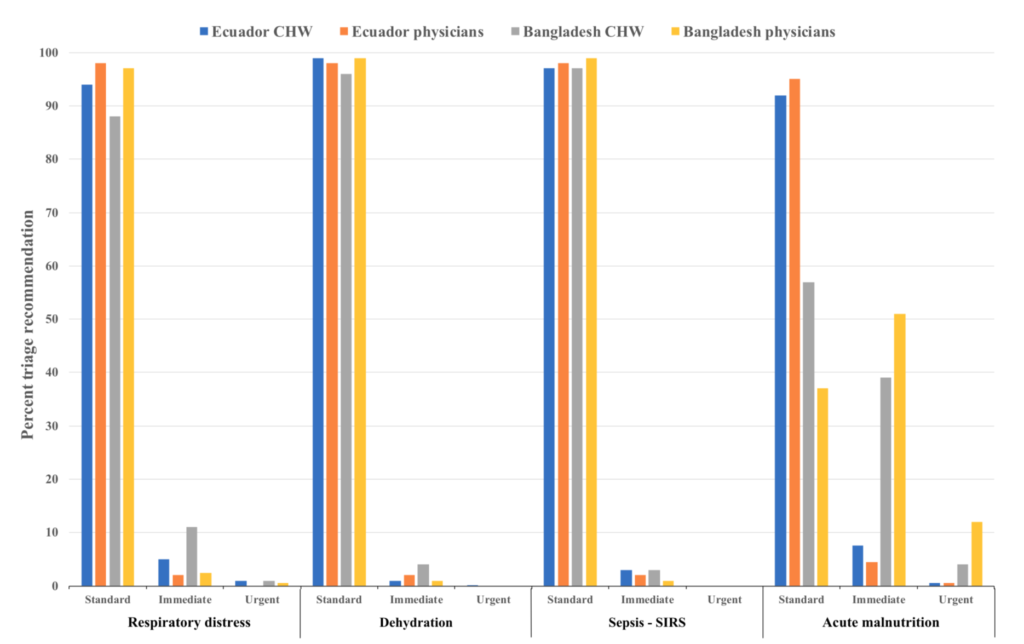
die each year from treatable clinical conditions such as pneumonia, dehydration secondary to diarrhea, and malaria. A majority of these deaths could be prevented with early clinical assessments and appropriate therapeutic intervention. In this study, we describe the development and initial validation testing of a mobile health (mHealth) platform, MEDSINC®, designed for frontline health workers (FLWs) to perform clinical risk assessments of children aged 2–60 months. MEDSINC is a web browser–based clinical severity assessment, triage, treatment, and follow-up recommendation platform developed with physician-based Bayesian pattern recognition logic. Initial validation, usability, and acceptability testing were performed on 861 children aged between 2 and 60 months by 49 FLWs in Burkina Faso, Ecuador, and Bangladesh. MEDSINC-based clinical assessments by FLWs were independently and blindly correlated with clinical assessments by 22 local health-care professionals (LHPs). Results demonstrate that clinical assessments by FLWs using MEDSINC had a specificity correlation between 84% and 99% to LHPs, except for two outlier assessments (63% and 75%) at one study site, in which local survey prevalence data indicated that MEDSINC outperformed LHPs. In addition, MEDSINC triage recommendation distributions were highly correlated with those of LHPs, whereas usability and feasibility responses from LHP/FLW were collectively positive for ease of use, learning, and job performance. These results indicate that the
MEDSINC platform could significantly increase pediatric health-care capacity in LMICs by improving FLWs’ ability to
accurately assess health status and triage of children, facilitating early life-saving therapeutic interventions.